Congratulations and welcome to Bristol, a fantastic city to study in and with endless fun to be had…Fresher’s week, parties, music venues, new friends, new surroundings and, last but not least, a new university course to get to grips with!
So before you get stuck in, get all your contraceptive needs sorted with us! We pride ourselves on being friendly and approachable and it’s all confidential so just book an appointment and come and talk to us.
So what are your options?
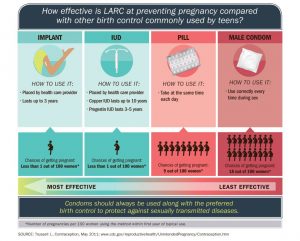
There are many different contraceptive methods available and you should choose one that suits you. Long Acting Reversible Contraception (LARC) has become a very popular option, especially for young adults.
We can provide LARC for free here at the SHS, as well as all the other contraceptive methods available.
All LARC is over 99% effective and they do not depend on you remembering to take them or use them to be effective…
Implants
- Small flexible rods inserted under the skin.
- Releases the hormone progesterone
- Stops ovulation & a fertilized egg implanting
- Prevents sperm reaching an egg
- Lasts for 3 years but can be removed earlier
- When removed, fertility will return to normal.
It’s a simple procedure that we can do at SHS and takes very little time. It also does not hurt to have it inserted or removed as we numb your arm!
The coil
There are two types of coil
The Copper Coil (IUD)
- Small plastic and copper device inserted into the uterus
- Prevents sperm reaching an egg
- May stop a fertilised egg implanting
- Lasts 5–10 years (depending on type) but can be removed earlier
- When removed, fertility returns to normal
Some women find their periods may be heavier or longer or more painful so it perhaps not the best choice for someone who already has problematic periods.
Mirena (IUS)
- Small, T-shaped plastic device inserted into the uterus
- Releases the hormone progesterone
- Prevents sperm reaching an egg
- Prevents fertilised egg implanting & may stop ovulation
- Lasts for for 5 years but can be removed earlier
- When removed fertility returns to normal.
Women usually find their periods usually become lighter, shorter and sometimes less painful and they may stop altogether after the first few months it has been inserted. A great option for those struggling with painful and/or heavy periods as well as a great contraceptive!
Injection
- Injection releases the hormone progesterone which works in same way as implant
- Lasts for 12 weeks (Depo-Provera)
- Periods may stop altogether or may become irregular.
Your periods and fertility may take time to return after you stop using the injection.
REMEMBER…Most methods of contraception DO NOT protect from STIs so use a condom if required!
We can provide these for FREE!
If you have had sex without contraception, or you think your method might have failed, please see us ASAP for emergency contraception.
If you think one of the above methods might be for you or you want to have a chat about other methods, please give our reception team a call, tell them what you want to discuss, and they can book you in with the right health care professional. Or you can use our on line booking system.
See you all soon!!